There are many different reasons why we experience back pain – one of them being spondylarthrosis. But what is behind this degenerative spinal disease, what are its causes and symptoms? And how can Akina help with treatment? Find the answers to these questions in this article.
What is spondylarthrosis?
The term spondylarthrosis is made up of the Greek words spondylos (vertebra) and arthros (joint) and refers to the wear and tear of the cartilage of the spine. Spondylarthrosis is a kind of degenerative spinal disease, the umbrella term is spondylosis or spondylosis deformans.
Development of spondylarthrosis
The cartilage surfaces of the small vertebral joints (so-called facet joints) are exposed to high weights throughout our lives. As we age or as a result of illness and injury, the ability of this cartilage to regenerate decreases, which leads to wear and tear of the joint surfaces. The wear and tear of the affected joints can lead to severe pain and reduced mobility of the back.
Under certain circumstances, spondylophytes, i.e. a kind of bony spines, form on the edges of the vertebral bodies. If these bony growths continue to spread and join together, they can lead to a change in the shape of the spine. Such a change increases stiffness and pain.
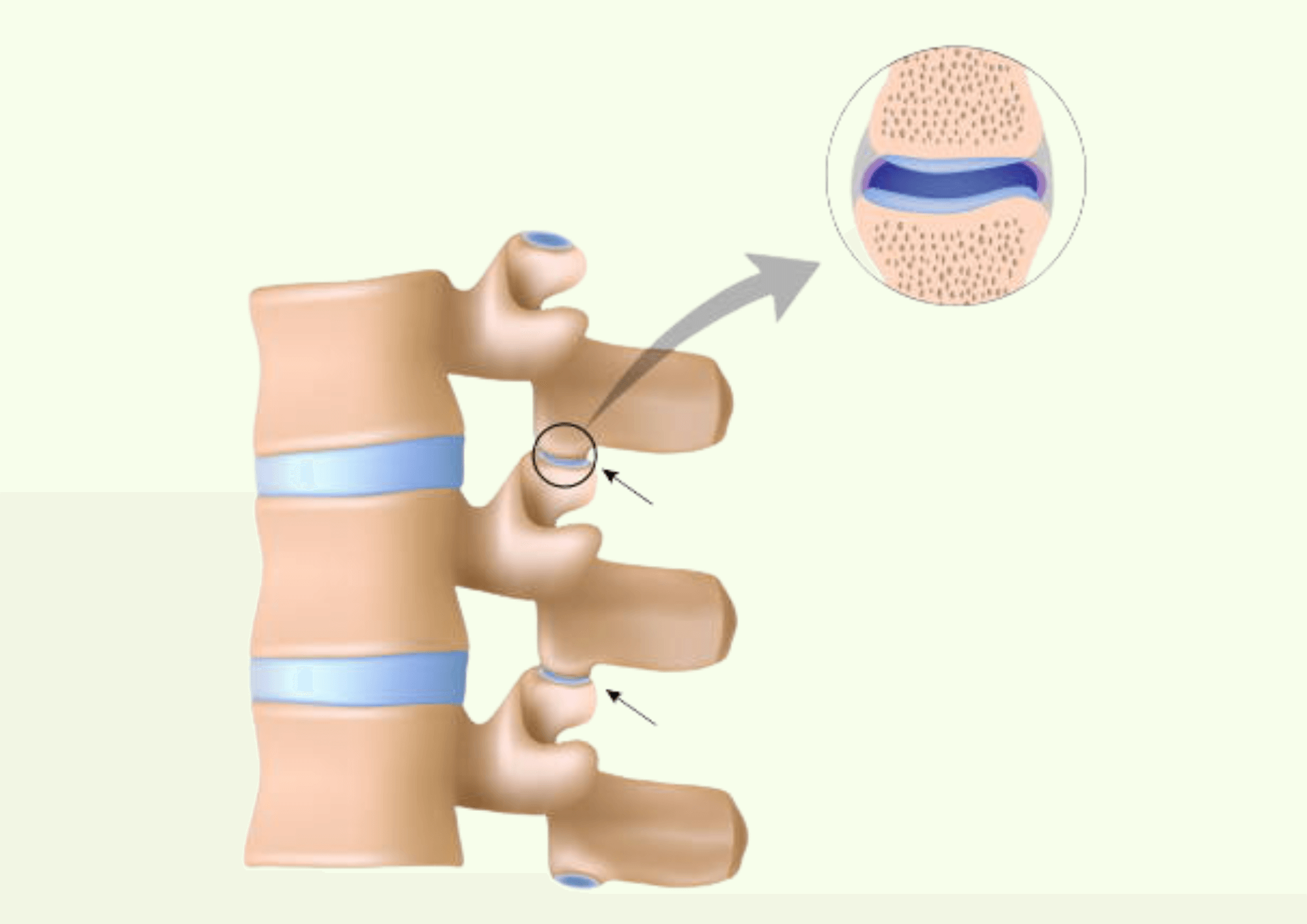
The facet joints are located at the articular processes of the individual vertebrae to connect them to each other. The joint is surrounded by a joint capsule, which contains nerve roots as well as the necessary blood supply. These are responsible for the perception of pain in this area.
Typical symptoms of spondylarthrosis
All areas of the spine can be affected by spondylarthrosis - if it is the cervical spine, neck pain occurs that can radiate into the arms. In the thoracic spine, it is mainly the middle and upper back that hurts. However, spondylarthrosis most commonly affects the lumbar spine, where it manifests in low back pain. The lumbar pain often radiates into the legs and intensifies when sitting and moving.
Regardless of which section of the spine the arthrosis occurs in, it often manifests itself in dull pain after standing up (so-called start-up pain), limited mobility and muscle tension. The back pain usually subsides at night, as the spine is relieved when lying down.
Common causes of spondylarthrosis
While spondylarthrosis is typically more common in older people, it can also affect younger people in some circumstances. Possible causes are
- Herniated discs
- Misalignments of the spine (scoliosis or Scheuermann's disease)
- Osteoporosis
- Lack of exercise, muscle weakness and obesity can also trigger or aggravate spondylarthrosis
The importance of exercise
Frequent, prolonged sitting and lack of exercise lead to an unbalanced load on the spine and the muscles that support and stabilize it lose strength. A lack of movement and the associated back problems often lead to poor or incorrect posture (e.g. hollow back), which in turn leads to further tension and pain.

Diagnosis and therapeutic measures for spondylarthrosis
Although the degenerative changes in spondylarthrosis cannot be reversed, the course of the disease can be positively influenced by a number of therapeutic measures. The primary aim is to relieve pain and maintain or restore mobility. A medical examination is essential to determine the correct diagnosis and appropriate treatment.
Diagnosis of spondylarthrosis
It is important that an orthopedic assessment is carried out early on in the case of back pain in order to define the causes and appropriate treatment methods. This is usually done by means of a physical examination: the doctor checks how flexible the spine is and at what point pain occurs. The exact localization of the pain is important for the diagnosis. Imaging procedures such as X-rays, an MRI (magnetic resonance imaging) or a CT (computer tomography) are carried out to detect herniated discs or bony changes in the vertebral joints. To ensure that the pain is actually coming from the facet joints and not from other structures such as the nerve roots or intervertebral discs, the affected joints may be anesthetized with a painkiller. If the patient is subsequently pain-free for a period of time, this is a strong indication of spondylarthrosis.
A timely medical examination can detect inflammation and associated pain as well as the development of movement restrictions at an early stage and slow them down. It is also important to recognize and avoid risk factors or aggravators of the disease. These include incorrect strain on the spine, obesity or weak back muscles.
Common therapeutic measures include:
- Exercise and physiotherapy
Sport and health-promoting exercise prevent a variety of back diseases – this also applies to spondylarthrosis. However, exercise is not only suitable for prevention, but also for treatment. Physiotherapeutic exercises can build up the back muscles, relieve pain and promote mobility.
When it comes to sports, the following generally applies: gentle sports such as swimming or cycling can be practiced with spondylarthrosis without any problems. However, patients must be cautious with impact sports such as tennis or volleyball, as well as weightlifting, as the sudden movements and heavy weights put abrupt and excessive strain on the intervertebral discs and facet joints.
- Healthy lifestyle
Not only exercise, but also a healthy, arthrosis-friendly diet, sufficient sleep and good management of everyday stressors are worthwhile in the treatment and prevention of back pain. - Anti-inflammatory painkillers
Non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac or ibuprofen can provide relief for acute, initial pain. If the pain is very severe, cortisone injections may be given under X-ray control. However, treatment with painkillers is rarely sustainable and is not suitable as a stand-alone or long-term therapy for spondylarthrosis. - Surgical interventions
If all conservative treatment methods have been exhausted, surgical measures can be resorted to. In a spinal fusion surgery (so-called spondylodesis), small implants are attached to the diseased part of the spine, which stiffen the vertebral bodies and adjacent small vertebral joints. The procedure serves to stabilize the spine and relieve back pain - however, it cannot lead to complete freedom from symptoms and can cause problems in the adjacent vertebral joints over the years. For these reasons, spondylodesis is only recommended if conservative measures are no longer sufficient or if the spondylarthrosis is accompanied by osteochondrosis (wear-related disease of the cartilage and bone) or spinal canal stenosis (narrowing of the spinal canal).

Akina: Your guide for at-home exercise therapy
When you have arthrosis, it can be difficult to stay active. You may ask yourself questions like: How much exercise is good for me with my condition? Which exercises are suitable for pain relief with spondylarthrosis? And which exercises will help improve my mobility and flexibility?
This is exactly what Akina is here for: our Akina Cloud software guides you through therapeutic training at home via our interactive, audiovisual platform. Instant AI feedback lets you know whether you are performing the exercise correctly and what you need to pay particular attention to during training. Physiotherapists have the opportunity to assess your progress or deficits and adapt your training plan accordingly. This allows patients and therapists to stay in dialogue and make physiotherapy - and thus the path to pain relief and restoration of mobility - more efficient.